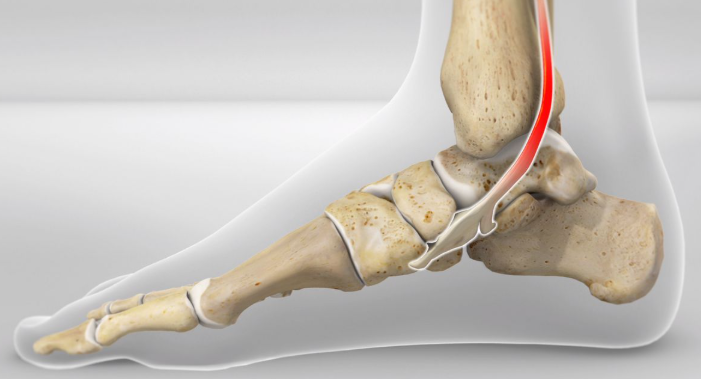
The tibialis posterior (TibP) muscle runs along the inside of your shin and down to your mid foot. It functions to invert and plantarflex the foot and control your arch. This means it plays a big role with walking, running and balancing.
TibP tendinopathy will present with pain and stiffness on the inside of your ankle and/or foot. There may also be swelling present. TibP tendinopathy pain will warm up with activity but often feels worse after a period of resting. It is typically associated with an increase of activity or a recent change in activity.
Examples might include:
– Someone who just took up running or increased their km per week
– An athlete bought a new pair of shoes for their sport
– A switch to synthetic turf when historically playing on grass
Tendons stem from our muscles which attach them to bone. Tendinopathy is considered an overuse injury of tendons. This means that the tendon is not coping with the demands that is being placed on it. This leads to pain and dysfunction of that tendon.
Assessment
Physiotherapists will ask about the history of the pain which will provide clues into whether it is or isn’t TibP tendinopathy.
A physical exam will also be performed which may include:
– Double or single leg calf raise
– Jumping or hopping
– Muscle strength testing
– Palpation of the lower leg
Imaging?
Imaging (ultrasound or MRI) is not typically required for accurate diagnosis of this injury. This is because imaging is poorly correlated with symptoms; a study found that under ultrasound imaging, 48% of people showed TibP tendinopathy despite have no medial foot or ankle pain (Mills et al., 2020).
Some people also present with normal imaging despite having clinical
features of TibP tendinopathy. Imaging is likely only required if your physiotherapist suspects a bony injury.
Treatment and Management
TibP tendinopathy can be successfully managed with physiotherapy. It may involve a period of relative rest and concurrent strengthening exercises of the TibP and other muscles in the body.
– Isometric ankle inversion
– Single leg calf raises
– Eversion
– Toe raises
– Energy storage and release exercises (hopping, depth jumps, lateral bounds etc)
– Strengthening of proximal muscles (hip and knee strength)
Other management strategies involve:
– Topical or oral NSAIDs (anti-inflammatory medication)
– Soft tissue release of TibP and other muscles in the lower leg
– Joint mobilisations
Differential Diagnoses – If it isn’t TibP tendinopathy, what else could it be?
– Deltoid ligament injury
– Navicular bone injury
– Flexor hallucis longus tendinopathy
– Tarsal tunnel syndrome